Pancreatic Cancer
The incidence of pancreatic cancer in India is 0.5– 2.4 per 100,000 men and 0.2–1.8 per 100,000 women. Pancreatic cancer is a disease of elderly, with most cases occurring in patients between 60 and 80 years of age. However, in India, the disease has an earlier age of onset with a median age of 52-55 years at presentation.
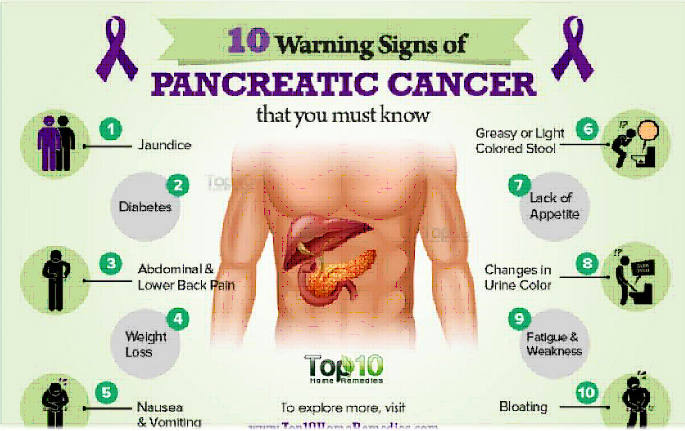
Signs and symptoms:
- Pain in the upper abdomen and back
- Loss of appetite and weight
- Yellowish discolouration of eye and
- skin(jaundice)
- Itching
- Fatigue
- Nausea and vomitting
- Changes in bowel habits
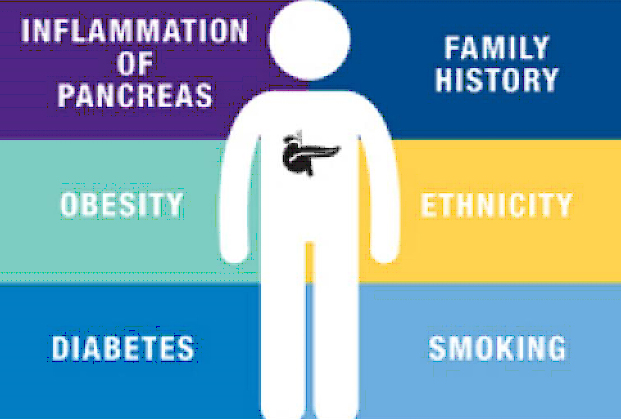
Risk factors:
- Smoking,Alcohol
- Diabetes
- Chronic pancreatitis
- Obesity
- Old age (>65 yrs)
- Family history of pancreatic cancer
Diagnosing pancreatic cancer:
Physical examination : Your doctor will examine your eyes and skin to look for signs of jaundice. Your doctor will also examine your abdomen to look for changes caused by the cancer.
Blood tests : Complete blood count, liver function test, renal function test, coagulation profile, CA19-9 (Tumor marker)
Radiological imaging: Ultrasound of the abdomen Pancreatic Protocol CT scan, PET-CT, .
In case of severely jaundiced patient, doctor might refer you to medical gastroenterologist for a ERCP and stenting to decompress the bile duct
prior to the surgery. Plastic or metal stents will be placed in your bile duct to relieve the obstructive jaundice.
Biopsy: Biopsy is not mandatory to diagnose the pancreatic cancer.
Most of the times diagnosis is confirmed by imaging tests. However, a small subset of patients with pancreatic cancer may present without jaundice. In these patients biopsy is required to confirm the diagnosis.
Management of pancreatic cancers:
Treatment options available for pancreatic cancer
- Surgery
- Chemotherapy
- Radiotherapy
- Combination of the above treatments
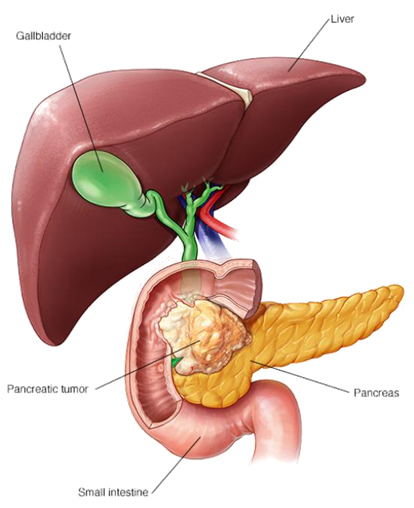
Surgery for pancreatic tumours:
Surgery for a pancreatic cancers depends on the location of the tumour
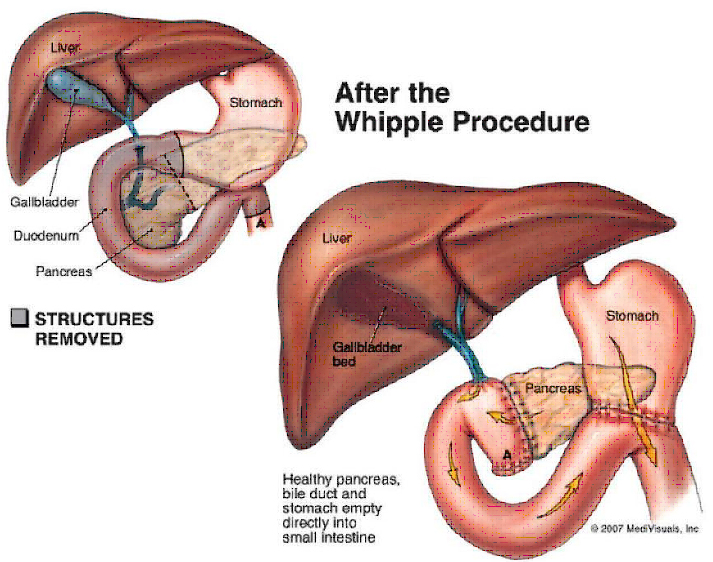
Surgery for periampullary and pancreatic head cancer: If the cancer is located in the periampullary and head of pancreas then the patient will require a Whipple’s procedure (pancreaticoduodenectomy),Whipple’s procedure is a technically very demanding surgery where the surgeon will remove the head of the pancreas, duodenum, gall bladder, common bile duct and regional lymph nodes. Following the removal surgeon reconnects the remaining pancreas, bile duct and stomach with the small intestine(jejunum). Thus providing pathway for food and bile. Post surgery patient will be monitered on daily basis. Patient will be on tube feeds for 2-3days, after which he or she will be slowly started on oral feeds. Recovery period is usually between 6-10days after surgery.
Surgery for pancreatic cancer of the body and tail :
For the tumours located in the body and tail of the pancreas requires distal pancreatectomy. Where in surgeon removes the body and tail of the pancreas. Some patients may require splenectomy( removal of spleen) as well. This is often done by laparoscopy or robotic techniques to minimize stay, less pain, early discharge from hospital and faster recovery.
Distal pancreatectomy and splenectomy
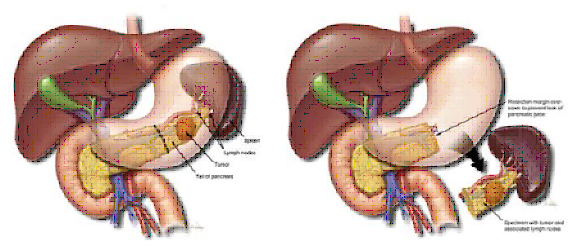
Complications os surgery includes bleeding, infection, collection inside the abdomen, nausea and vomiting. Complication rates have come down with better understanding of the disease and improved technical skills. Complication are fewer when its done by a experienced surgeon and in a high volume centre.
Patients who require splenectomy along with distal pancreatectomy will have to receive pneumococcal, H influenza and meningococcal vaccine to prevent post splenectomy infections.
Chemotherapy for pancreatic tumours:
Chemotherapy has been shown to extend life for people with pancreatic cancer. It is often combined with surgery or radiation therapy for tumors confined within the pancreas. It used as a primary treatment for inoperable tumors that are confined within the pancreas. It is used for people with pancreatic tumors that have spread from the pancreas to other parts of the body. If patient requires surgery plus chemotherapy then the timing of chemotherapy may be prior to surgery (neoadjuvant) or after the surgery (adjuvant) based on the extent of disease . Some patients may require both neoadjuvant plus adjuvant chemotherapy.
Radiotherapy for pancreatic cancer:
Radiation therapy in pancreatic therapy may be used combination with chemotherapy and surgery to completely eliminate tumors that are contained within the pancreas and any remaining cancer cells. It is also given to shrink locally advanced tumors so that surgery can be performed safely and to relieve pain and other symptoms of metastatic disease
Palliative care in pancreatic surgery :
Palliative care is an option for patients who are in advanced stages of pancreatic cancer, who are deemed inoperable. In these patients aim of the treatment would be to get relief from the distressing symptoms. For example palliative stenting to relieve the obstructive jaundice, which will provide a pathway for bile and relive the patient of itching symptoms and cholangitis
-
Can pancreatic cancers be prevented?You may not be able to prevent the pancreatic cancer, but you can lower the risk rates by practicing healthy diet, physical exercise, maintaining proper weight, avoiding smoking and alcohol
-
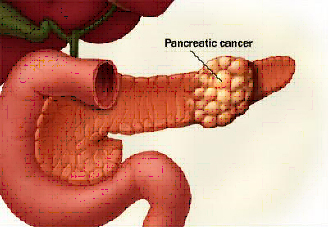
What causes pancreatic cancer?Currently, it isn’t known what causes pancreatic cancer, however, we do know that cancer occurs when cells develop mutations in their DNA. These mutations cause the cells to grow rapidly and uncontrollably, eventually forming a tumor
-
What is the life expectancy of a person post whipple’s procedure?Life expectancy after a whipple’s procedure depends on the final histopathology report . In Periampullary cancers, is 40% to 60 % and in cancers involving head and uncinate process of pancreas the survival rate is approx. 30 to 40 %.Some patients may require adjuvant chemotherapy and radiotherapy which prolong their survival rate
-
Is there a screening test for pancreatic cancer?Despite of being one of the leading cause of cancer deaths around the world there is no reliable screening test for pancreatic cancer
-
Is there a relationship between diabetes and pancreatic cancer?There is no association between type1 diabetes and pancreatic cancer, but there is mounting evidence regarding association between type 2 diabetes and pancreatic cancer
-
What are the side effects of radiotherapy and chemotherapy?Radiation therapy may cause patients to become very tired as treatment continues. In addition, when patients receive radiation therapy, the skin in the treated area may sometimes become red, dry, and tender. Radiation therapy to the abdomen may cause nausea, vomiting, diarrhea, or other problems with digestion. For most patients, the side effects of radiation therapy go away when treatment is over.Patients who undergo chemotherapy may also be more likely to get infections, bruise or bleed easily, and may have less energy. Other side effects such as poor appetite, nausea and vomiting, diarrhea, or mouth sores.Usually, these side effects go away gradually during the recovery periods between treatments or after treatment is over.