Cytoreductive Surgery
What is Cytoreductive Surgery?
Cytoreductive Surgery (CRS) is a complex surgical procedure primarily used in the treatment of certain advanced cancers that have spread to the peritoneum (peritoneal carcinomatosis ) . The aim of this surgery is to remove all the tumors from different regions of the abdominal cavity which may include multiorgan resection. This procedure is often combined with other treatments, such as HIPEC and systemic chemotherapy to improve outcomes.
- When combined with hyperthermic intraperitoneal chemotherapy (HIPEC), cytoreduction therapy is beneficial in cases of cancer that has developed or spread to the abdominal cavity, such as appendiceal cancer, pseudomyxoma peritonei, colon cancer, gastric cancer, ovarian cancer, and peritoneal mesothelioma.
- These therapies are administered in the following order: cytoreductive surgery, followed by HIPEC to destroy any residual microscopic cancer cells.
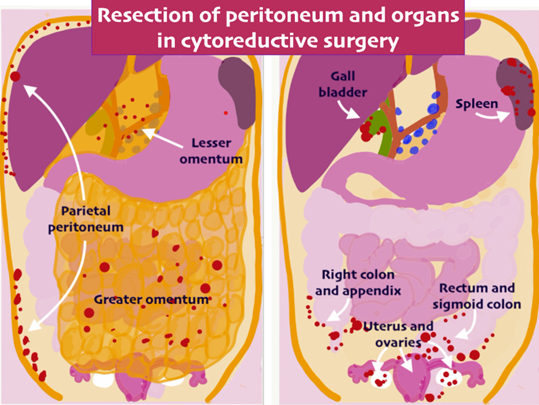
- Before taking up a patient for surgery, detail assessment of scans is done to evaluate the extent of the disease and calculate PCI and to assess the operability. The expertise of the surgeon to remove all the tumor deposits is key to the success and long term outcomes after CRS. The organs are removed in a way that is compatible with normal life after surgery.
- Many a times, Diagnostic Laproscopy is performed to visualise the peritoneum. As scans may not detect nodules which are less than a cm, laproscopy will help us to evaluate those small nodules and also allow us to see certain key areas inside abdomen which will decide the operability. When complete removal of the tumor seems unlikely, surgery is not undertaken.
- Cytoreductive surgery removes the visible components of the tumor, leaving only the microscopic cells remaining. If the tumor has spread into other organs, it may be necessary to surgically remove those organs in order to free the affected area of the tumor. Some of the organs that may be removed include the gallbladder, spleen, a portion of the small or large intestine, and the lining of the abdominal wall (peritoneum). In most cases, removal of these structures does not have any long term impact on the patient’s quality of life and after complete recovery, most patients lead a normal life.
- HIPEC involves the administration of a heated chemotherapeutic solution to the abdomen in order to destroy any residual malignant cells. The heated chemotherapy is more effective at penetrating tissues and killing cancer cells while minimizing systemic side effects. When the treatment is completed, the chemotherapy solution is emptied from the abdomen and the incision is closed using sterile equipment.
- The heated solution is kept around 42-43°C. This increases the penetration and the efficacy of the chemotherapy.
- The surgery is highly intricate and may take several hours (sometimes over 10 hours) to complete. It requires a specialized surgical team with experience in handling such extensive procedures.
- Patients with peritoneal carcinomatosis (disease that has spread in the peritoneal cavity) are seldom recommended surgery because they are thought to have unresectable disease, or cancer that cannot be removed surgically. However, CRS has been shown to be effective in some patients with peritoneal carcinomatosis especially in mucinous tumors as they are not very chemosensitive. Proper sequencing is required to get the best results. It may be combined with chemotherapy either before or after CRS to improve outcomes. important link

Conditions Treated with CRS and HIPEC
- Peritoneal Carcinomatosis: Spread of cancer within the abdominal lining caused by gastrointestinal or gynecological cancers.
- Appendiceal Cancer: When the tumor is confined to the appendix, it may mimic acute appendicitis. Sometimes it is detected during surgery as a perforation with mucin in entire abdomen or as a mass on CT scan. When widespread, it presents as a pseudomyxoma peritonei.
- For low grade tumours, when it is confined to the appendix, patients will have to undergo surgery to remove the appendix and/or right colon. In the majority of the patients with tumors of the low grade variety, removal of the colon is not required and removal of the appendix alone is sufficient ( also depends on the final histopathology report ) . For High Grade tumors, removal of the appendix and right colon is required.
- For patients in whom the tumor has spread to the peritoneal cavity, the combined approach of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (HIPEC) is the most effective and beneficial treatment. This combined approach has improved long term outcomes.
- Colorectal Cancer ( With metastasis to the peritoneum) : These cancers are treated with a combined approach of systemic chemotherapy , CRS and HIPEC. (sequence may change ). The PCI score also tells us about the prognosis. The less the score, the better the outcome.
- Ovarian Cancer: In cases where cancer has spread extensively within the abdominal cavity.
- Mesothelioma: Rare cancer affecting the peritoneum.
- Gastric cancer : In selected patients with low PCI.
Benefits of CRS with HIPEC
- Targeted Treatment: Delivers chemotherapy directly to the affected area, minimizing systemic side effects.
- Improved Outcomes: Combined surgical and chemotherapy approach enhances long-term outcomes though this can vary depending on the extent of the disease and surgery.
- Reduced Recurrence Rates: Effectively targets residual microscopic cancer cells to lower the risk of recurrence.
Cytoreductive Surgery Risks : Infection , bleeding, delay in bowel activity, generalised weakness. Some patients may have deranged renal function.
Postoperative care and Recovery: Patients require close monitoring in the ICU for a day or two following surgery. Cytoreductive surgery with HIPEC takes 6-10 hours to complete. Depending on the type of cancer, the patient had to stay in the hospital for 7-10 days or longer. The healthcare staff urges the patient to keep a balanced combination of rest and exercise. While the patient may feel fatigued for about 2-3 months, subsequent to this, patients can get back to a normal life. Stoma therapist will help to educate the patient and the family about stoma care.