Colorectal Cancer
Most colorectal cancers are "silent" tumors. They grow slowly, and you may not notice any symptoms until they’re large. But you can take some steps to prevent colorectal cancer, and you can cure it if you find it early. It’s important to have regular screening exams to spot cancer or precancerous areas, especially if you have a high risk of getting it. The lifetime chance of developing colorectal cancer is 1 in 22 for men and 1 in 24 for women
Colorectal Cancer Risk Factors
Things that can raise your chances of getting it include:
- A personal or family history of colorectal cancer or polyps
- A diet with a lot of red and processed meats
- Inflammatory bowel disease such as Crohn's disease or ulcerative colitis
- Conditions passed down through your family, such as familial adenomatous polyposis (FAP) and hereditary nonpolyposis colon cancer (HNPCC)
- Obesity
- Smoking
- Lack of activity
- Heavy alcohol use
- History of Polyps in colon
Colorectal Cancer Symptoms
In some cases, you might not notice any signs of colorectal cancer. When you have them, they can include:
- A change in your bowel habits that doesn’t go away, such as constipation or diarrhoea
- Incomplete evacuation of stools
- Bleeding from your rectum
- Blood in your stools
- Abdominal discomfort
- Nausea and Vomitting
- Weight loss with no clear cause
- Significant fall in hemoglobin (anemia)
- Weakness or fatigue
- A lump in your abdomen or rectum
Colorectal Cancer Diagnosis
Your doctor will do physical exam ination ,feel your abdomen for any swollen organs or masses. They might also order one or more of these tests to find the cause of your symptoms :
- Rectal exam: Your doctor can use their fingers to feel for growths.
- This is the standard screening test that experts recommend. Your doctor uses a thin, flexible tube called a colonoscope to look at your entire colon and rectum.
- Biopsy: Your doctor may take out a bit of tissue during a colonoscopy or sigmoidoscopy and send it to a lab for testing. They can also use a needle to take a sample, with a CT scan or ultrasound to guide them. Complications are rare, but you may have some bleeding or discomfort.
- Imaging tests: PET – CT scan is done to map the disease, see for spread to distant organs and stage your disease. MRI is more useful for rectal cancers to assess local staging.
Colorectal Cancer Treatment Options
Treatment will depend on many factors. You and your doctor should consider:
- The stage of the disease
- How well certain treatments will work for you
- Your overall health
- The risks and side effects
- How much the treatment costs
- The option would prefer after thorough discussion.
You might have one or more of these treatments:
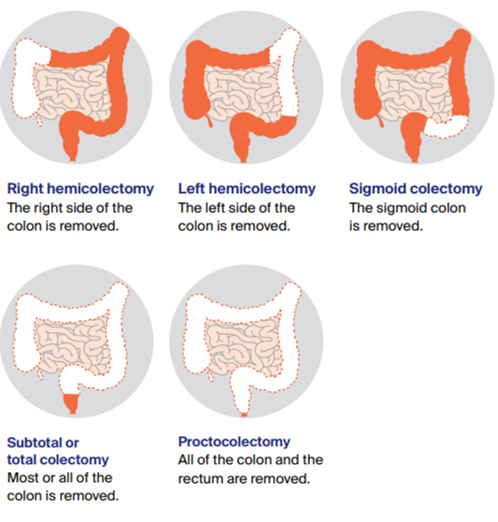
Surgery
Surgery is the most common initial medical treatment for colorectal cancer. During surgery, the tumor, a small margin of the surrounding healthy intestine, and adjacent lymph nodes are removed. In patients with rectal cancer, the rectum sometimes is permanently removed if cancer arises too low in the rectum. The surgeon then creates an opening (colostomy) on the abdominal wall through which solid waste from the colon is excreted. Specially trained nurses (enterostomal therapists) can help patients adjust to colostomies, and most patients with colostomies return to a normal lifestyle.
Surgery can be either minimally invasive in the form of Robotic/ Laproscopic or Open surgery. Extent of surgery depends upon the location of tumor. It usually involves removal of affected segment of large bowel followed by anastomosis (joining) of healthy segment of intestine. Evidence has shown that there is rapid recovery, less pain, early return to work when it performed with minimally invasive approach. Also oncologic outcomes are equivalent in both open and minimally invasive approach.
In Rectal cancers, Surgery can be either Anterior Resection (AR) , Low AR, Intersphicteric resection or Abdomino perineal resection depending upon the location of the tumour. Patients may have a temporary stoma in AR, Low AR or ISR to divert the stools and give time for the joint to heal which is usually done with staplers. Patients who undergo APR, will have a permanent stoma.

Chemotherapy
Chemotherapy drugs destroy cancer cells or stop them from spreading. You can take the medicines in pill form or through an IV. There are many types of these drugs. Some work better together, so you may take two or more at the same time. You usually get these drugs in the form of cycles every 2 or 3 weekly depending upon the type of drugs and dose of drugs.You might have chemotherapy after surgery or you could have it before surgery to make a tumor smaller and easier to remove. And it's often the best way to slow the spread of the disease.
Radiation therapy
Radiation therapy uses high-energy X-rays, electron beams, or chemical agents called radioactive isotopes to attack cancer. The radiation is aimed directly at the tumor. New techniques and machines have reduced toxicity of radiation to the surrounding tissues. It damages chromosomes in cancer cells so they can't multiply. Its use as primary treatment has been limited to treating cancer of the rectum, either in the form of short course RT or long course RT, before /during/after chemotherapy depending upon the location of the tumour from the anal verge and its local stage.
Follow-Up Care
After you’ve finished your treatment for colorectal cancer, follow-up care is very important. Regular checkups can help find any changes in your health, and if the cancer comes back (or “recurs”), it can be treated as soon as possible.
You will be required to undergo :
- Clinical examination
- Blood tests and Tumour markers - CEA levels which can help us to identify early recurrence.
- Imaging : CT scan Thorax, Abdomen and pelvis at regular intervals.
Colorectal Cancer Prevention
- Healthy tobacco-free lifestyle
- Exercise and healthy lifestyle (The American Cancer Society and says adults should get 150 minutes of moderate-intensity or 75 minutes of high-intensity exercise (or a combination of these) each week.
- Low-fat, high-fiber diet that includes at least 2 1/2 cups of fruits and vegetables each day
- Cut back on red meat and other high-fat foods
- Avoid overcooking or barbecuing meats and fish.
- Screening for colorectal cancer
- Genetic counselling and testing
Genetic counseling and testing
- Families with multiple members having colon cancers, multiple colon polyps, cancers at young ages, and other cancers such as cancers of the ureters, uterus, duodenum, and more, may take advantage of resources such as genetic counseling, followed possibly by genetic testing. Genetic testing without prior counseling is discouraged because of the extensive family education that is involved and the complicated nature of interpreting the test results.
- The advantages of genetic counseling followed by genetic testing include:
(1) identifying family members at high risk of developing colon cancer to begin colonoscopies early
(2) identifying high-risk members so that screening may begin to prevent other cancers such as ultrasound tests for uterine cancer, urine examinations for ureter cancer, and upper endoscopies for stomach and duodenal cancers
(3) alleviating concern for members who test negative for the hereditary genetic defects.